To answer this question, we need to first clarify exactly what a DNR is and what it is not. DNR stands for Do Not Resuscitate. It’s also known as a DNRO (Do Not Resuscitate Order), “no code” or “allow natural death”. A DNR is not the same as a living will. It only covers the specific circumstance of providing cardiopulmonary resuscitation or advanced cardiac life support when someone’s heart or breathing stops.
Who would have a DNR?
Generally, the DNR is signed by the doctor as part of the medical treatment plan. It can apply in hospitals, care facilities and at home/in the community. Facilities may have their own additional forms and steps to take. A DNR is typically for patients who are terminally ill, suffering from an end-stage condition or a persistent vegetative state.
The DNR is much different from a living will, which is often done by healthy persons as part of their advanced care planning. The living will deals with different aspects of end-of-life care. Because it is a real-time medical order, a DNR would typically not be in place for a healthy person who would likely wish to be resuscitated.
A patient may not want CPR attempted when:
- Medical benefit is unlikely. CPR is not likely to be successful (or prolong life very long) for those who are terminally ill or have severe health issues.
- Quality of life would suffer. Sometimes CPR is only partly successful, particularly for frail elderly. Though the patient survives, they may suffer damage to the brain or other organs. Or, they may become dependent on a machine to breathe.
- Death is expected soon. Patients with a terminal illness may decide to allow the natural process of dying rather than being resuscitated.
It is important to talk to your healthcare professionals about your situation. Whether you could benefit from resuscitation depends on your condition and many factors. Your personal beliefs about dying and life-sustaining treatments play a role too. And, the DNR is only one small aspect of end-of-life care decisions. Therefore, the conversations should cover different scenarios and aspects of planning.
Legal Details about the DNR
The legalities surrounding DNRs vary by country and state. In Florida, Chapter 64J-2.018, Florida Administrative Code, addresses the Do Not Resuscitate Order. Chapter 765 of the Florida Statutes deals with various end-of-life issues. The Florida law specifies that the DNR form must be printed on yellow paper. Also, if you have a DNR in another state, it won’t be accepted in Florida. Check out the Florida Department of Health’s FAQs on DNRs to learn more.
Understanding CPR
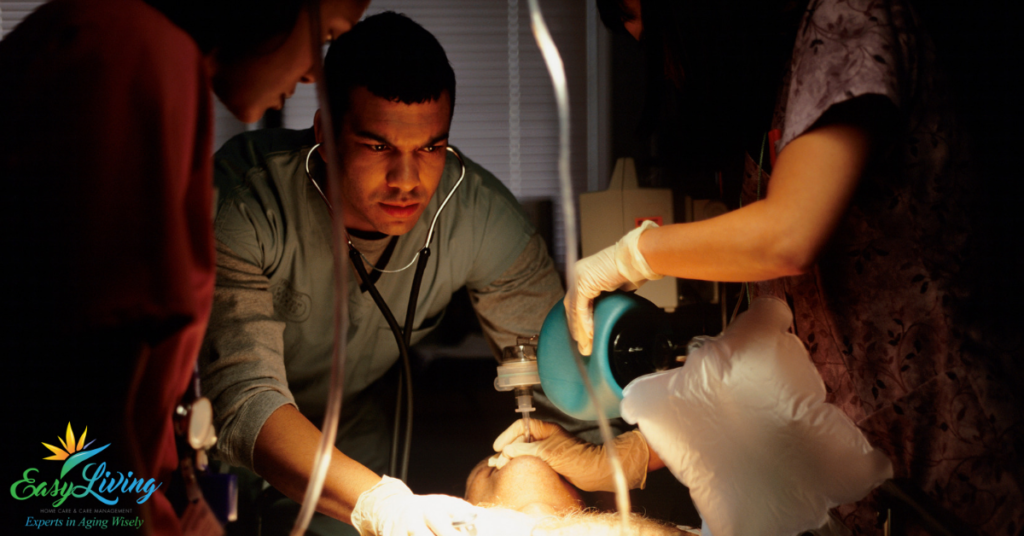
In addition to the basic CPR we may all be familiar with, more advanced techniques include:
- Intubation- The insertion of a tube into the mouth or nose to help with breathing.
- Mechanical Ventilation- The use of a machine to move air into the lungs.
- Medications- Intravenous drugs might be given to help with blood pressure regulation, heart rhythm, and blood flow.
- Cardioversion – The use of a controlled electrical shock to change heart rhythm.
Figures vary and best practices are improving outcomes. However, research suggests that 10-20% of all people who get CPR will survive and recover enough to leave the hospital. For chronically ill elderly patients, some studies have shown a less than 5% chance of surviving long enough to leave the hospital. This doesn’t mean that CPR isn’t a valid choice. It just emphasizes the importance of understanding the realities. It is vital to talk to your healthcare providers about your condition.
We feel it is reckless not to have these conversations and understand more. For example, in one study when participants (older adults 85+) were made aware of their likelihood to survive, only 6% chose to have CPR. Many people don’t understand all the implications and their choices.
When might it be risky not to have a DNR?
It all goes back to what you want, and being actively involved in your medical decision making (or having someone do so on your behalf). Resuscitation can be risky if you’re unlikely to benefit but might suffer deteriorated quality of life. It can also put you (or more likely your family) in a tough situation when you require continued artificial measures to prolong your life. If you have a living will and have decided you do not want such measures, resuscitation may trigger what you’d hoped to avoid.
It can be psychologically and financially costly to get resuscitated in these conditions. And, without a DNR guiding them, medical personnel must proceed with resuscitative efforts.
Also, if you do not wish to be resuscitated, make sure you have executed a DNR properly. First, it must be done properly and next it must be accessible when needed. It needs to be on your medical record at the hospital, care facility or with your home health provider. If you are in the community, rescue workers will typically look on the refrigerator door (must be on yellow paper). The Florida law also provides for a “patient identification device”, an added option that can travel with the patient. Detach it from the form, laminate it and wear it around the neck, for example.
Action Steps
- Complete advance care planning. Execute (and update) documents such as a living will and healthcare surrogate. Talk to your family members/designated decision makers about your wishes. Set an appointment to talk to your doctor about your condition and wishes. Discuss whether a DNR is appropriate for you or will be at some stage.
- Meet with a healthcare advocate. They can help you organize your medical records and advance directives, talk to healthcare providers, and navigate the medical system. It is so helpful to have a sounding board for tough decisions and thinking through all aspects.
- Make sure all your advance directives are accessible and provided to your healthcare team. Our team can help with getting everything set up properly, as well as making referrals to professionals such as elder law attorneys.
- Get our free Aging Wisely Checklist for tips and tasks at different stages.